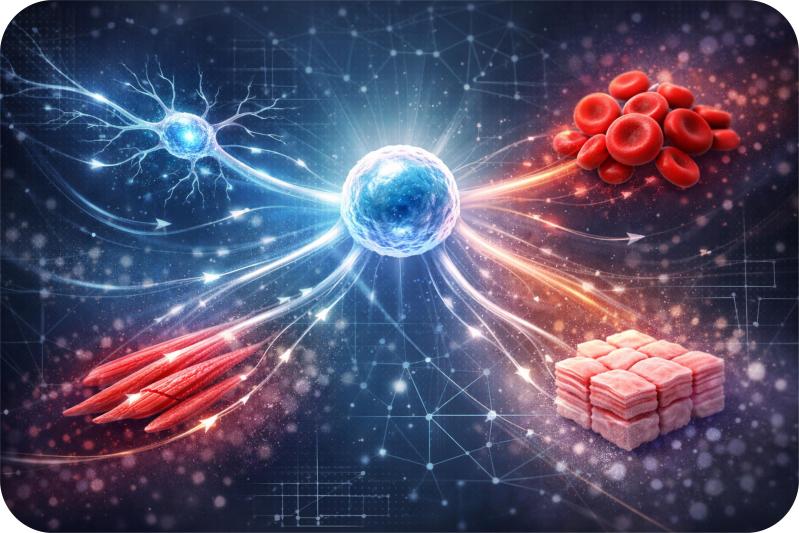
The advancement in science and technology have made possible for humans to tackle life-threatening diseases to highly intricate surgeries. Medical science has reached a mark where it has potential to create artificial organs for transplant, saving millions of lives. And now researchers have discovered a way to create human blood, using stem cells.
Supported by the funds provided by the Wellcome Trust, Professor Marc Turner and his team from the University of Edinburgh have found a process to produce human blood on an industrial scale. Researchers believe that with the new process, they can produce and stock, disease free type O red blood cells, ready to be used in transfusion. As per the National Institutes of Health, millions of Americans every year require blood to be used to replace blood lost during surgery or an injury or for transfusion during disease like anemia, hemophilia, thalassemia and so on.
The research team has formulated a rewinding technique in which they culture regular red blood cells derived from humans and converted them into stem cells, termed as induced pluripotent stem cells (iPS). These stem cells, under specific biochemical environment (similar to conditions in the human body), grow into mature Type O blood cells. Researchers specifically chose to create type O blood, considering the fact that is a universal donor blood group.
The team plans to test the technique in humans in the clinical trials that would be conducted in the year 2016 or 2017. The artificial blood would be used for transfusion, required by the patients suffering from a blood disorder, thalassemia. The behavior of artificial blood cells will then be observed.
Other researchers have also attempted to create synthetic blood, however, Prof Turner and his team is the first to devise a technique to produce high quality blood that meet all the safety standards required for blood transfusion in humans.
If the clinical trials yield result as expected, the technique can then be used to manufacture limitless supply of type O blood, disease free and compatible with patients. Post 1980s, blood banks has taken up measure to closely screen, all the blood from HIV and Hepatitis B infections, ensuring them to be completely safe for transfusions. But there are many countries where still these blood screening standards are not met.
But producing the artificial blood on an industrial scale is still a challenge, says Prof Turner. Each unit of blood compromises of almost a trillion red blood cells and therefore, creating laboratory like conditions on an industrial scale to meet the demand is still a major challenge.
Under laboratory conditions, transfusion of single blood unit requires around £120. The cost can be reduced, if the team can formulate a plan to scale up the production. This would help to save patients who mostly face tough time as the required type of blood is not accessible at the right time and the right place.
Hopefully very soon the factory made blood will be available in the blood banks, saving lives of millions across the world.